Introducing the Emergency Medicine Rotation Exam, Perfect for PA Students
Rosh Review, LLC is not sponsored or endorsed by, or affiliated with, the Physician Assistant Education Association. All trademarks are the property of their respective owners.
Announcing the newest Rotation Exam – Emergency Medicine module, available to Physician Assistant students and programs. This module is best suited for PA students looking for a focused, high-yield review for the PAEA Emergency Medicine End of Rotation™ exam. It joins our growing list of Rotation Exams, including Rotation Exam – Family Medicine, Rotation Exam – Internal Medicine, Rotation Exam – Psychiatry & Behavioral Health, Rotation Exam – General Surgery, and Rotation Exam – Women’s Health. This content is novel and not included in Rosh Review’s PANCE Qbank, Mock exams, or Power Packs.
The Rosh Review Rotation Exam for Family Medicine is compatible with the PAEA published content blueprint.
Categories include the following:
- Cardiovascular (20%)
- Orthopedics/rheumatology (15%)
- Pulmonology (10%)
- Gastrointestinal/nutritional (10%)
- ENOT/ophthalmology (7%)
- Neurology (8%)
- Dermatology (5%)
- Urology/renal (6%)
- Hematology (4%)
- Psychiatry/behavioral medicine (5%)
Content is organized by task:
- History and Physical (15%)
- Diagnostic studies (10%)
- Diagnosis (25%)
- Health maintenance (10%)
- Clinical intervention (10%)
- Clinical therapeutics (10%)
- Scientific concepts (10%)
Here is an example:
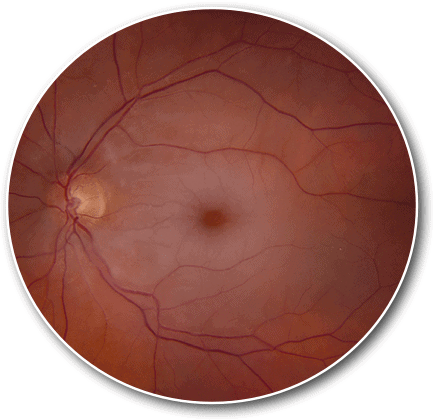
A 77-year-old woman presents to the ED with acute painless vision loss. On funduscopic exam, you note the above. Which of the following is the most likely diagnosis?
A. Central retinal artery occlusion
B. Central retinal vein occlusion
C. Idiopathic intracranial hypertension
D. Optic neuritis
Answer A
This patient is exhibiting signs and symptoms of central retinal artery occlusion. Central retinal artery occlusion is defined by the occlusion of blood flow to the retina, typically by emboli from the carotid artery or from the heart in patients with atrial fibrillation. Risk factors for central retinal artery occlusion include hyperlipidemia, coronary artery disease, atherosclerosis, hypertension, diabetes, and glaucoma. Signs and symptoms include sudden, painless, complete loss of monocular vision. Physical exam will reveal an afferent pupillary defect or Marcus Gunn pupil, which is a pupil that will have a normal consensual light response followed by a paradoxical dilatation with direct light exposure. Diagnosis is on funduscopic examination as you will see a boxcar appearance of the retinal vessels due to interruption of the blood flow and a pale retina with a cherry red spot on the fovea. Management of central retinal artery occlusion involves a multi-pronged approach. Ophthalmology should be consulted immediately upon suspicion of the diagnosis. Orbital massage may be used to attempt to dislodge the clot. Anterior chamber paracentesis may also be attempted. Pharmacologic agents may be used such as acetazolamide, mannitol, or timolol in an attempt to decrease intraocular pressure.
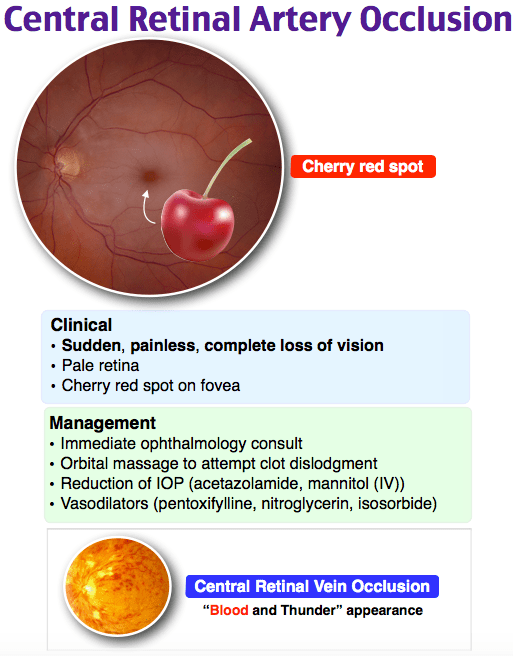
Central retinal vein occlusion (B) will have the appearance of “blood and thunder” on funduscopic exam with retinal hemorrhages and cotton wool spots. Idiopathic intracranial hypertension (C) will have the appearance of papilledema on funduscopic exam and is often bilateral. These patients will typically have headaches and incomplete vision loss. Optic neuritis (D) may or may not have evidence of optic disc hyperemia and inflammation on funduscopic exam and is typically painful.
One Step Further question:
What systemic neurologic disorder is associated with optic neuritis?
Answer:
Multiple sclerosis.
Since these categories and tasks are integrated into our improved performance and feedback page, you have access to robust data to help you fine-tune your studying.
Study on…
The Rosh Review Team
A bolus of confidence. A lifetime of knowledge.





Comments (0)