How to Use the Frances Guide Qbank to Pass Your Adult-Gerontology Acute Care (AGACNP) Certification Exam
Everyone who passed the Adult-Gerontology Acute Care (AGACNP) Certification Exam knows that one of the best resources is the Frances Guide.
Ahh…the Frances Guide. What is it?
Many years ago, someone who took the AGACNP Certification Exam documented the most important topics students needed to know to help them prepare for the exam. Basically, everything you need to know to pass the exam is found in the AGACNP Frances Guide. Well, almost everything. You’ll still need to do a general review after reviewing the Frances Guide, but this guide is one of the best places to start to identify most of the topics on the exam.
What is the most important way to use the Frances Guide?
In addition to reviewing the Frances Guide, it is critical that you use the Francis Guide Qbank to truly learn the material to pass the AGACNP Certification Exam.
What is the Frances Guide Qbank?
Take all of the content from the AGACNP Frances Guide and turn it into questions and comprehensive explanations, and you’ve got the Frances Guide Qbank. This Qbank allows you to benefit from retrieval practice and the testing effect to get the best chance of passing the AGACNP Certification Exam.
See for yourself:
A 36-year-old man presents to the emergency department with complaints of abdominal pain and diarrhea that started 1 week ago. He reports no significant prior medical history. On physical exam, he is tender to palpation in the left lower quadrant of his abdomen. Plain radiographs of the abdomen show thumb printing in the transverse colon. Based on the information provided, what does the thumbprint sign suggest?
A. Inflammation
B. Intraluminal gas
C. Normal anatomy
D. Obstruction
Answer A
The thumbprint sign describes thumb-shaped, nodular indentations projecting into the lumen, generally occurring at regular intervals. Its appearance is commonly seen on radiographs or computed tomography of the large intestine and is consistent with bowel wall thickening and edema. This sign most commonly occurs secondary to an infective or inflammatory process within the bowel. It may be seen in inflammatory bowel disease, colitis, diverticulitis, or ischemic bowel. While it is considered a nonspecific finding, its presence offers an immediate identification of an inflammatory process, allowing for empiric treatment to start earlier than if waiting on diagnostic testing results to process.
Intraluminal gas (B) appears as rounded bubbles on abdominal imaging demonstrating the presence of air. Based on the information provided, this is not the most appropriate answer choice. Normal anatomy (C) will have identifiable haustra (sacculations made from the longitudinal and circular muscles) on imaging with intermittent gas patterns and fecal material. Obstruction (D) may show up as dilated bowel loops with or without fluid but are not always visible on X-ray imaging. Based on the information provided, this is not the most appropriate answer choice.
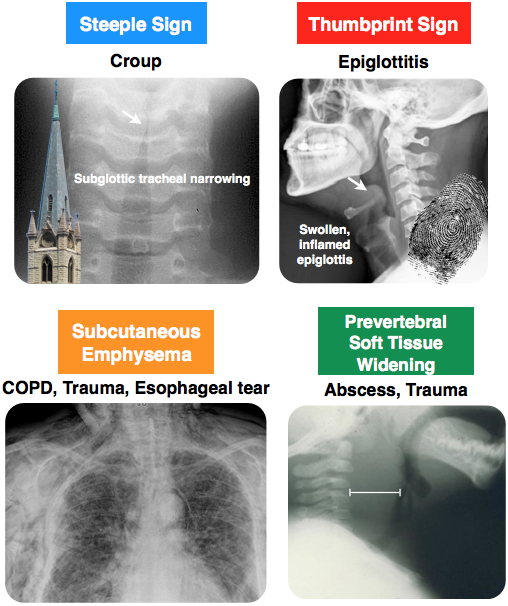
Rapid Review: Epiglottitis
- Patient will be complaining of rapid onset of fever and dysphagia
- PE will show patient leaning forward, drooling, inspiratory stridor
- Imaging will show thumbprint sign
- Most commonly caused by Strep and Staph species, H. influenzae (prior to the Hib vaccine)
- Treatment is IV antibiotics and airway management
Here’s another question from the Frances Guide Qbank:
A 46-year-old woman is examined in the recovery unit after a total abdominal hysterectomy. She is complaining of pain, blurred vision, and photophobia in the left eye. She states that she “feels like there is sand in my eye.” Which of the following is the gold standard for diagnosing the suspected condition?
A. Fluorescein dye examination
B. Optical coherence tomography
C. Tonometry
D. Transillumination test
Answer A
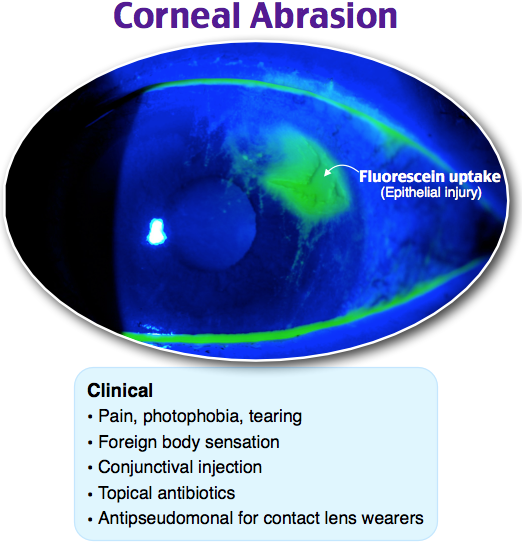
The gold standard for diagnosing corneal abrasion is a fluorescein dye examination. During this test, fluorescein (an orange dye) is applied to the eye through a drop, then the eye is examined under a blue light. Scratches to the cornea and foreign bodies can be detected using this test. Symptoms of corneal abrasion include eye pain, watering, decreased visual acuity, photophobia, redness, and sensation of a foreign body. Corneal abrasions should be treated with topical fluoroquinolone drops or ointments four times daily. Most corneal abrasions heal within 2–3 days. Complications of corneal abrasion include corneal ulcer, bacterial keratitis, recurrent erosion, and traumatic iritis.
Optical coherence tomography (B) measures the thickness of the retinal nerve and is helpful in diagnosing several eye conditions, such as glaucoma, optic neuritis, macular degeneration, and diabetic retinitis. Tonometry (C) measures the pressure inside the eyes. It is used to diagnose glaucoma. A transillumination test (D) is used for the diagnosis of hydrocele. A light is shown through the scrotum and, if positive, will show fluid around the testicle.
Rapid Review: Corneal Abrasion
- Patient will be complaining of pain, photophobia, tearing, or foreign body sensation
- Diagnosis is made by fluorescein stain
- Treatment: Most are self-limiting, antipseudomonal for contact lens wearers
Let’s go for a third example! Here’s another from the Frances Guide Qbank.
A 72-year-old woman presents to the intensive care unit with headache, lightheadedness, increasing confusion, and lethargy. Imaging reveals a chronic subdural hematoma with 11 mm clot thickness and minimal midline shift. Which of the following is the most appropriate next step?
A. Consult neurosurgery for surgical evacuation
B. Order strict bedrest with head of the bed flat
C. Prepare for intubation
D. Start seizure prophylaxis
Answer A
Chronic subdural hematoma is a collection of blood on the surface of the brain below the dura. While more common in the older population, risk factors include alcohol use disorder, seizures, coagulopathies, cerebrospinal fluid shunts, and patients who are higher fall risks. While chronic subdural hematomas may start out as acute subdurals (such as with trauma from a head injury), the bleeding that leads to chronic formation is often secondary to small veins that slowly leak. Symptoms may be minor, such as headache, confusion, transient-ischemic attack-like symptoms, or language difficulties or may progress in severity to coma, seizures, and hemiplegia. Imaging with a noncontrast computed tomography of the head will determine the diagnosis. For patients with mild symptoms, monitoring closely is recommended. Seizure prophylaxis is used by some but can be safely discontinued after 1 week if no seizure activity is noted. Coagulopathies should be reversed if present. Consult with neurosurgery for surgical evacuation of the hematoma is indicated if there is significant progression of focal deficits or moderate to severe mental status changes, if the thickness of the subdural has progressed to ≥ 10 mm, or if midline shift is ≥ 5 mm. Patients will have clinical improvement if approximately 20% of the collection is removed, resulting in close to zero subdural pressure. Residual subdural fluid collections are common and do not warrant repeat surgery unless they increase in size.
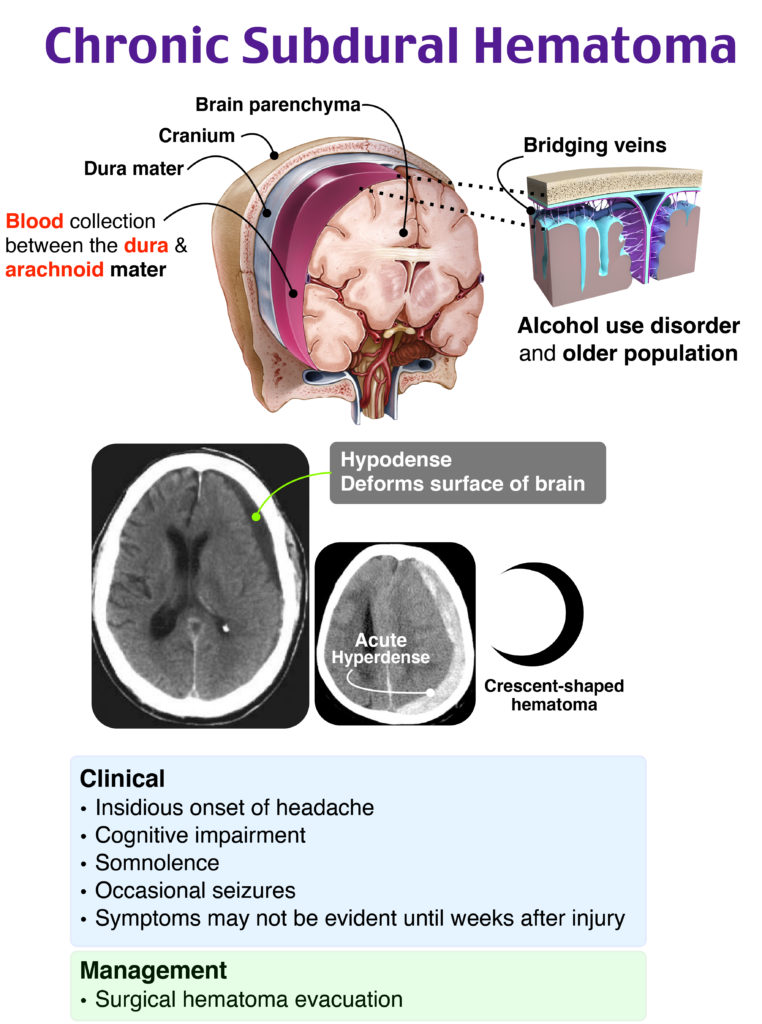
Order strict bedrest with head of the bed flat (B) for 24–48 hours is appropriate following surgical drainage of subdural hematoma to prevent reaccumulation of blood at the surgical site. As the patient in the vignette has not yet had surgery, this is not the most appropriate answer choice. Prepare for intubation (C) is only appropriate if the patient has respiratory decline, which has not been documented in this vignette. Respiratory status should be closely monitored, however, as it can occur rapidly with continued compression on the brain and associated midline shift. Start seizure prophylaxis (D) is recommended by some, particularly if seizures have occurred, but given the information in the vignette, this is not the most appropriate answer choice.
Rapid Review: Subdural Hematoma
- Patient will be an older adult or chronically use alcohol
- With a history of a fall or traumatic head injury
- Complaining of headache, mental status changes, seizures, or focal deficits
- Diagnosis is made by noncontrast CT, will appear as crescent-shaped hematoma
- Most commonly caused by rupture of the bridging veins
- Management includes neurosurgical consultation
Be ready for your AGACNP Certification Exam. You’ve worked hard, and your patients expect the best from you.
Important links:
The Frances Guide
The Frances Guide Video Review
The Frances Guide Qbank





Comments (0)