Podcast Ep 35: Shigellosis, Ischemic Colitis, Suicide, & More
Reach for it. Push yourself as far as you can.
-Christa McAuliffe
Welcome back to Roshcast Episode 35! It was great chatting with a bunch of listeners at ACEP last week. We received a lot of excellent feedback.
This week, we’ll be doing a couple of diarrhea questions to link up with the last EM Clerkship episode, in addition to a few randomly generated questions. Don’t forget that we are still running a trauma ring tone contest. Listen closely for a ring tone in an upcoming episode and e-mail us at roshcast@roshreview.com or tweet to us at @Roshcast the exact time of the ring tone to win a prize, which will certainly come in handy as we get closer to the in-training exam. Let’s get started with a review from recent posts on the Rosh Review Blog.

- Pterygium is a fleshy triangular growth from the medial canthus towards the cornea. They are usually slow growing and seen in those with excessive sunlight exposure. They are managed with artificial tears.
- Pterygium typically doesn’t require surgery but may need excision if it is causing a visual disturbance. Make sure the patient is already following with an ophthalmologist or give them a referral if needed.
- Retinal detachments present with painless loss of vision, floaters, flashing lights, or as a curtain lowering sensation. On physical, you may see a hazy gray retina with whitish folds.
- The most common location for an ectopic pregnancy is the fallopian tube.
Now onto this week’s podcast
Question 1
A 2-year-old girl presents after a witnessed seizure. The parents state that she has not been to daycare in two days, as she has bloody diarrhea and a fever. Her vitals on presentation are T 103.1°F, HR 167/min, BP 73/43 mm Hg, RR 48/min, and oxygen saturation 96%. Currently, the patient has a normal neurologic exam and minimal abdominal tenderness. There are no rashes. Labs show a WBC of 19,000, and urinalysis reveals an elevated specific gravity. Which of the following is the most appropriate next step in management?
A. Acetaminophen for fever and follow-up with primary care provider
B. Blood and stool cultures, IV antibiotics, and admission
C. Neurology consultation and admission
D. Oral antibiotics and follow-up with primary care provider
Question 2
An 82-year-old nursing-home resident is sent to the emergency department with lower abdominal pain and bloody diarrhea. He has a history of vascular dementia, hypertension, and hyperlipidemia. On examination he is afebrile, and a nasogastric aspirate is negative for evidence of bleeding. Which of the following is the most likely cause of this patient’s bleeding?
A. Angiodysplasia
B. Diverticular bleeding
C. Ischemic colitis
D. Peptic ulcer disease
Question 3
Which of the following is considered a risk factor for suicide?
A. Female sex
B. First-trimester pregnancy
C. First year of marriage
D. Recent incarceration
Question 4
Which of the following scenarios is most appropriate to safely discharge home a 2-year-old who has swallowed a coin?
A. The child is not drooling
B. The child is tolerating oral sips and the parents are reliable
C. The coin is in the stomach
D. The coin is oriented in the sagittal plane at the level of the clavicular heads
Question 5
A 35-year-old-man with a history of occasional bloody diarrhea and abdominal pain presents with acute onset severe abdominal pain. Vital signs are significant for a temperature of 39°C, heart rate 140/min, and blood pressure 82/55 mm Hg. On physical exam, his abdomen is distended and tympanic. Which of the following diagnostic studies is indicated first at this time?
A. Abdominal radiograph
B. Barium enema
C. CT scan of the abdomen pelvis with IV contrast
D. Sigmoidoscopy
Question 6
A 45-year-old woman complains of two days of fluctuating diplopia and dysphagia. Her exam reveals a left cranial nerve VI palsy, ptosis, and proximal muscle weakness in her extremities. What is the pathophysiology of her disease?
A. Antibodies to the acetylcholine receptor at the neuromuscular junction
B. Inhibition of acetylcholine release at the synapse
C. Mutation of superoxide dismutase causing cell death
D. Reduced number of dopamine receptors in the midbrain

- Patients with Shigella often present with fever, abdominal cramps, and diarrhea with mucus or blood. Infants with Shigella are also at risk for seizures.
- Shigellosis should be treated supportively. Patients who are immunocompromised, have bacteremia, attend daycare, or live in a nursing home require treatment with antibiotics. Children should be treated with ceftriaxone, 50 mg/kg in a once-daily dose up to a max of 1.5g for 5 days.
- Ischemic colitis is caused by inadequate blood flow through the mesenteric vessels. It often affects the watershed regions.
- Ischemic colitis can be treated supportively with bowel rest and IV fluids unless there are signs of peritonitis or infarction.
- Risk factors for suicide include male sex, age, history of mental illness, personal or family history of a suicide attempt, poor financial situation, unemployment, poor physical health, being Caucasian, and isolation.
- With respect to suicide, marriage, and first-trimester pregnancy are both protective.
- Swallowed foreign bodies that do not pass through the esophagus, which occurs 2% of the time, have a risk for esophageal perforation or erosion.
- Emergent endoscopy is indicated if the swallowed foreign body is a battery, is sharp, or if there are signs of obstruction.
- Coins in the sagittal plane on X-ray are more likely to be in the trachea than in the esophagus.
- Toxic megacolon presents with colonic dilatation and systemic toxicity. Patients usually present after having symptoms of colitis for several days.
- If there is concern for toxic megacolon, an abdominal X-ray should be the first imaging study to look for colonic dilatation, to a diameter greater than 6 cm.
- Toxic megacolon can be precipitated by IBD, pseudomembranous colitis, CMV colitis, and bacterial colitis.
- Myasthenia gravis is caused by antibodies to the acetylcholine receptor at the neuromuscular junction.
- Ptosis and diplopia are the most common first symptoms of a myasthenic crisis. This is followed by proximal muscle weakness, dysphagia, and dyspnea. Respiratory failure can be seen in the later stages.
- Myasthenia gravis can be diagnosed by the edrophonium or Tensilon test.
- Myasthenia gravis can be treated with plasma exchange and IVIG. Ice decreases symptoms but is not a permanent solution.
That wraps up Episode 35. Don’t forget to follow us on Twitter @Roshcast and @RoshReview. We can also be reached by email at roshcast@roshreview.com and are open to any feedback, corrections, or suggestions. You can help us pick questions by identifying ones you would like us to review. To do so, write “Roshcast” in the submit feedback box as you go through the question bank. And finally, if you have a minute, make sure to rate us and leave comments on iTunes to help spread the word about Roshcast.
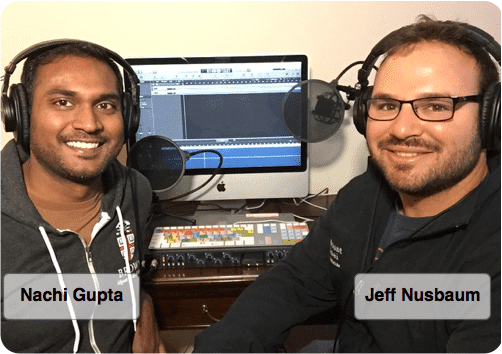
Until next time,
Jeff and Nachi





Comments (0)