Podcast Ep 42: Korsakoff Syndrome, AAA, Prolapsed Umbilical Cord
The secret of change is to focus all of your energy, not on fighting the old, but on building the new.
–Socrates
Welcome back to RoshCast for Episode 42! With the in-training exam around the corner, go back and power through old episodes during commutes to pick up as many points as possible. Good luck!

- Patent ductus arteriosus (or PDA) closes, the neonate will present in heart failure and shock.
- Turner’s syndrome is associated with coarctation. Turner’s is also associated with webbed neck, short stature, and low-set ears.
- Individuals with Turner’s syndrome are missing an X chromosome as well, making it a 45,XO chromosomal condition.
- A blood pressure differential between the arms and legs—specifically, the pressure in the arms is higher than the legs. Depending on the specific anatomy, you might even note a difference in the pressures between both arms.
- Classic EKG and chest X-ray findings associated with coarctation of the aorta include left ventricular hypertrophy and rib notching, respectively.
Now onto this week’s podcast
Question 1
Which of the following is typically seen in Korsakoff syndrome?
A. Cerebellar dysfunction
B. Long-term memory impairment
C. Ophthalmoplegia
D. Recent memory impairment
Question 2
Which of the following is the most common physical exam finding in an abdominal aortic aneurysm?
A. Abdominal bruit
B. Diminished femoral pulses
C. Duodenal obstruction
D. Pulsatile abdominal mass
Question 3
A 24-year-old woman at full term presents with rupture of membranes and contractions. Sterile exam reveals a crowning infant with a visible cord. After elevating the fetal head, what management is indicated?
A. Clamp and cut cord and proceed with delivery
B. Continue with standard delivery
C. Emergent cesarean section
D. Intravenous tocolytics
Question 4
You suspect a 35-year-old man has epiglottitis with impending airway compromise. Which of the following is the best method for confirming the diagnosis?
A. Computed tomography of the neck
B. Frontal cervical soft tissue radiograph
C. Indirect laryngoscopy
D. Lateral cervical soft tissue radiograph
Question 5
A 21-year-old man presents with a stab wound to the right chest. His vitals are HR 157/min, BP 81/43 mm Hg, RR 28/min, and oxygen saturation 91%. The patient is intubated, and packed red blood cells are started. Physical examination reveals a bleeding wound to the right chest, a midline trachea, and decreased breath sounds on auscultation of the right hemithorax. Which of the following should be performed next?
A. Application of a pelvic binder
B. Placement of a right thoracostomy tube
C. Right chest thoracotomy
D. Transfer to operating room
Question 6
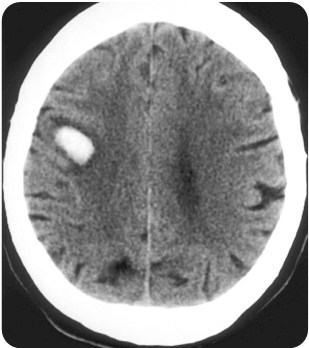
A 65-year-old man with a history of hypertension presents with left-sided weakness beginning two hours prior to arrival. Vitals are BP 155/85 mm Hg, HR 102/min, RR 12/min, oxygen saturation 100% on RA. His CT scan is shown above. Which of the following therapies is appropriate?
A. Antihypertensives to lower mean arterial pressure by 25%
B. Head of bed at 30°
C. Neurosurgical evacuation
D. Prophylactic antiepileptic drugs

- Korsakoff syndrome is a chronic neurologic disease caused by thiamine deficiency that typically presents with impairment of recent memory formation. Patients may also exhibit apathy and confabulation.
- Wernicke’s encephalopathy often presents with ophthalmoplegia, nystagmus, ataxia, and mental status changes. Wernicke’s encephalopathy and Korsakoff syndrome or often seen simultaneously.
- Treat both Wenicke and Korsakoff syndromes with thiamine and magnesium.
- The most common physical exam finding in AAA is a pulsatile mass. At a diameter of 5 cm, the risk of rupture increases markedly. Diagnosis is made by ultrasound or CT scan.
- For umbilical cord prolapse during delivery, plan for an emergent C-section. If C-section is not possible, attempt manual replacement of the cord into the uterus, followed by rapid vaginal delivery.
- Epiglottitis classically presents with rapid onset of fever and dysphagia, often with drooling, anxiety, stridor, and a muffled voice.
- The best method for confirming the diagnosis of epiglottitis is via indirect laryngoscopy, which can be done with a nasopharyngoscope. However, be careful as manipulation can lead to laryngospasm and airway obstruction. Make sure a surgical airway kit is available at the bedside.
- The classic finding on lateral neck X-ray in those with epiglottitis is a thumbprint sign.
- An ED thoracotomy would be indicated in a patient who loses vitals in route to the hospital or in the ED.
- For intracranial hemorrages, treatment is first supportive with airway protection and maintenance of adequate perfusion. Elevate the head of the bed to 30 degrees and maintain normothermia, normocarbia, and euglycemia. Current data do not support the use of antiepileptics.
That wraps up RoshCast Episode 42! Be sure to also check out RoshCast blog for questions from this episode and prior episodes, related images and tables, as well as bonus teaching points. There are also tons of other great free resources there to help prepare you for the boards and the wards. Don’t forget to follow us on twitter @RoshCast and @RoshReview. And you can always email us at RoshCast@RoshReview.com with any feedback, corrections, or suggestions. You can also help us pick questions by identifying ones you would like us to review. Write “RoshCast” in the submit feedback box as you go through the question bank. Lastly, if you have a minute, make sure to rate us and leave comments on iTunes to help spread the word about RoshCast.
Good luck on the in-training exam next week!
Jeff and Nachi





Comments (0)