ECG Tips for Physician Assistants: A Tutor’s Guide

Although I have been a certified PA for almost 15 years, I remember those dreaded feelings of anxiety towards EKGs like it was yesterday. Sure, I understood the science, and even read a much-recommended resource on the topic by Dr. Dale Dubin, but putting that knowledge into practice was something else altogether. How did one read and interpret an EKG? I didn’t know how to tackle the problem. It seemed like an insurmountable mountain.
Unfortunately, it was a mountain I had to climb. In multiple clinical medicine courses like Cardiology and Emergency Medicine, the EKG was a major part of the coursework. And yet the more I worked at it, the more it seemed to elude me. This was a problem, because I needed to know the EKG to not only get through PA school, but also do well on my End of Rotation Exams and prepare for the PANCE!
Sound a little (or maybe a lot) like your own struggles? Take heart—there was a solution to be found! One of my mentors helped me TREMENDOUSLY by teaching me the five steps to reading and interpreting EKGs. And yes, I would be happy to pay the information forward to you as a virtual mentor!
By the way: If you are interested in EKG interpretation 2.0, check out this great article by Dr. Rosh!
The ABCs of EKGs
Let’s start by considering what an EKG is. Essentially, an EKG is a mechanical analysis of the dynamic physiology of the heart.
A bit of a history lesson for you: in 1887, Augustus Waller used a mercury capillary electrometer and observed deflections of the mercury that indicated electrical activity in the heart. Using Waller’s discovery, Willem Einthoven built a modified version of the mercury capillary electrometer and recorded the activity of the heart in an improved way. He developed a string galvanometer, which can be seen in this article from NCBI.
Of course, since Einthoven, there have been many changes to his design that have dramatically improved cardiac care. However, we still thank you, Einthoven!
Why Should PA Students Learn to Interpret EKGs?
As a PA student and future certified PA, your ability to successfully read and interpret EKGs is tantamount to effective practice as a clinician, especially if you work as a cardiology PA, emergency medicine PA, or even as a surgical PA (as they are obtained for preoperative consultations).
If you apply the following 5 Steps, it greatly improves your interpretation, but it really ensures you don’t miss anything on the EKG, as there are multiple “look-alikes” and otherwise hidden nuggets of valuable data that can be easily missed. However, if you follow the steps, you will be less likely to miss those important nuggets!
Alright, now that we’ve set things up, let’s move on to the how and why of the five steps to reading and interpreting EKGs like a cardiologist!
The 5 Steps to Reading and Interpreting EKGs
1. Is the rhythm regular or irregular?
Most EKGs indicate a regular heart rhythm. Observe the QRS complex; moreover, focus on the upward positive deflection, this is the “R” portion of the QRS. These are usually the easiest to identify on an EKG.
I’ll bet you didn’t know that well before I became a PA, I was a DJ! When examining an EKG, be like a DJ: look for the discernable “marching” of beats. If you can appreciate a regular beat—it is regular!
Pro tip: when starting out, consider using calipers to observe the distance between the “R” portion of the QRS. If you don’t have calipers, place a piece of paper just below the Rs and make a mark under subsequent ones. If they appear the same distance, you are regular!
For irregularities, you will not be able to march out Rs!
2. What’s the rate?
The normal rate is between 60-100 bpm. Always remember this!
With a regular rhythm, there are two methods to determine the heart rate using a given EKG (whether a 12-lead full EKG or a rhythm strip).
The first is the counting of large boxes. Starting with an R wave that best lines up with a solid (dark) red line, count the lines between until you reach the next R wave. The rates start at 300 bpm with line 1, then 150 bpm with line 2, 100 bpm with line 3, and so on. Here is a very helpful graphic to help you learn the rates:
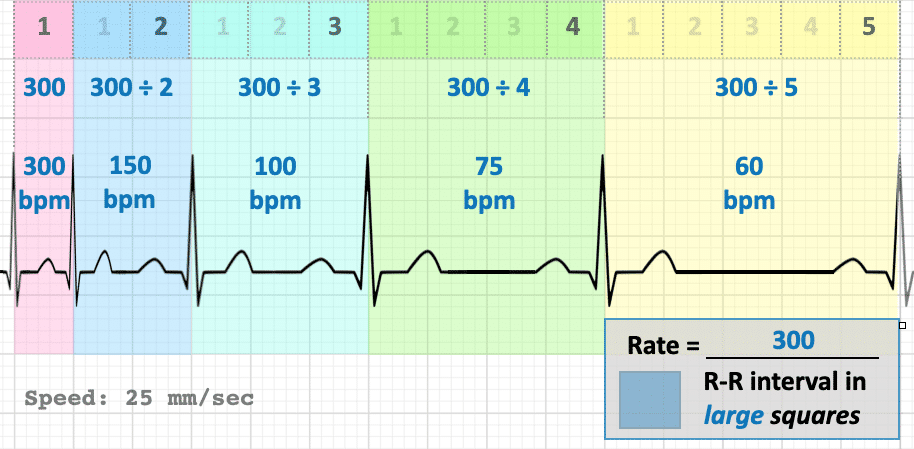
I would commit them to memory. Do a couple of practice tracings to get this down pat!
For regular (or irregular) rhythms, there is another method. If you consider a typical 12-lead EKG or rhythm strip, the amount of time across the entire thing is usually 6 seconds. You can count the number of QRS complexes that you see in the strip, and multiply by 10. This will give you a 60-second timeframe of beats. For example: if you count 10 QRS complexes in 6 seconds, you have a rate of 60 bpm! (Is this correct?)
3. What do the P waves and the PR intervals look like?
After determining the rhythm and rate, look at the appearance of the P wave. This is referred to as the morphology (i.e., what does it look like). The P wave represents atrial depolarization (and contraction). It should appear like a small round mound. Here are some examples of abnormal appearing ones and their interpretations.
Additionally, are the PR intervals normal? A PR interval should be a flat line leading from the end of the P wave to the beginning of the QRS. It is normal if it’s less than 0.20 seconds. This is equal to five smaller boxes (or less).
If it is abnormal or there are specific changes, this may indicate a heart block or even a condition called WPW (if it appears short).
4. What do the QRS complexes, ST segment, and T waves Look Like?
The QRS complex represents the depolarization of the ventricles. It should be less than 0.12 seconds (3 small boxes or less).
Is it “tight,” which means the rhythm is being generated by the sinoatrial (SA) node? Or, does it appear wide, which is known as aberrancy? Aberrancy refers to a situation in which the rhythm is likely being generated below the AV node (in the ventricular area). The ST segment is a subject for an entire blog post on its own!
Bottom line: a normal ST segment should be flat. If it is elevated, there is a myocardial infarction (heart attack) or if it is depressed there is ischemia (a lack of normal blood flow).
As for the T wave, it represents the repolarization of the ventricles. It should have a gradual hump appearance, not a flipped one. If it is, this may be another sign of ischemia. If it is peaked, the patient may have hyperkalemia (too much potassium in the blood).
5. Interpretation
Here is where all of the data you’ve obtained leads to your diagnosis. Pro tip: if everything is normal, you are looking at a normal sinus rhythm!
Further Reading
For further info, the resource by Dr. Dale Dubin is The Rapid Interpretation of EKGs. It’s very well written and an invaluable resource for learning EKGs!
Additionally, Dr. Adam Rosh compiled an additional list of resources in his blog post mentioned above.
Psst! If you’re also interested in learning ECG interpretation based on both single-concept and case-based questions from an online Qbank, take a look at the Clinical ECG Qbank.
Please do not hesitate to reach out to the fabulous, experienced tutors at Blueprint Prep for all of the mentoring you need to become an expert on EKGs!
To your success,
Frank Ritz, PA-C, DScPAS, MPAS
Blueprint Test Prep Tutor
Rosh Review is the leader in online test preparation with board exam review for PA students, programs, and PA-Cs across the U.S. Learn more about Rosh Review’s PA-C Qbanks for the PANRE, PANRE-LA, CAQs, and more.





Comments (0)