The First Med-Peds Qbank to Help You Pass Your Internal Medicine and Pediatrics Board Exams
To prepare for your boards as a Med-Peds resident, you may feel like you have to recreate the wheel to craft your study plan. As if one board exam isn’t enough, you face the challenge of finding two great study resources to ace your exams. But the more time you spend searching for multiple board review resources, the less time you have to learn the material and feel confident on exam day. Now, with the Rosh Review Med-Peds Qbank, you can start learning (and stop searching) right away.
How Do You Choose a Qbank?
Previously, you might have considered the MKSAP, NEJM Knowledge Plus, or UWorld for internal medicine. For pediatrics, you might have considered PREP, MedStudy, or BoardVitals. Rosh Review’s Med-Peds Qbank gives you access to both the Internal Medicine and Pediatrics Qbanks, which you can easily toggle between with customized dashboards. This means you have access to more than 5,000 questions and comprehensive explanations based on the ABP and ABIM content blueprints, so you can create your study schedule around your two board exams and seamlessly switch between specialties.
How to Study for the Internal Medicine and Pediatrics Boards with a Qbank
First things first, how should you study for your boards? With so much content to cover, we recommend targeting your “unknown unknowns.” These are concepts you don’t know (and don’t even know they exist). How do you determine them? Like this:
- Answer a question from the Qbank you’re focusing on (internal medicine or pediatrics)
- If you answer incorrectly, read the explanation
- Take notes about why the correct answer is correct, and make sure to take notes on anything in the explanation that you didn’t already know (be sure to keep your notes organized by topic)
If you do this for every question you answer incorrectly, and if you regularly review your notes and add information to topics as you do more questions, you’ll eventually determine your unknown unknowns. In return, you’ll uncover most of your blind spots that questions on the boards can ask about.
When you’re balancing studying for two board exams, set a consistent study goal (such as getting through X questions per week from the relevant Qbank, aiming to complete at least 1,000 to 2,000 questions to prepare for your exam). This can help you set aside plenty of time to determine your unknown unknowns and feel confident on exam day.
Now let’s take a look at some of the content found in the Med-Peds Qbank.
Internal Medicine
A 74-year-old woman with a history of polymyalgia rheumatica and hyperlipidemia presents to the emergency department with crushing substernal chest pain. Her ECG demonstrates ST elevations in leads I, aVL, V2–V3, and V5–V6, with reciprocal ST depression in II, III, and aVF. She is taken emergently to cardiac catheterization, where a drug-eluting stent is placed in her left anterior descending artery. She is started on aspirin 81 mg, clopidogrel 75 mg, and metoprolol succinate 25 mg daily. Her home medication, simvastatin 10 mg, has been changed to atorvastatin 40 mg daily. She is also on prednisone 5 mg daily for her history of polymyalgia rheumatica. Echocardiogram on hospital day 2 demonstrates a left ventricular ejection fraction of 55% and no wall motion abnormalities. Her vital signs are currently stable. What is the best medication to prescribe next in the management of this patient?
A) Digoxin 0.125 mg daily
B) Pantoprazole 40 mg daily
C) Rivaroxaban 2.5 mg twice daily
D) Sacubitril-valsartan 24 mg/26 mg daily
Answer B
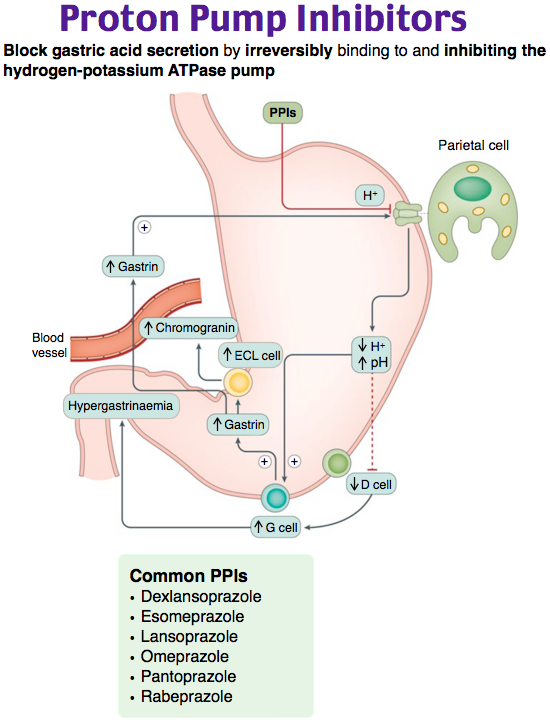
Starting the patient on pantoprazole 40 mg daily is the best management at this time. This patient with an ST segment elevation myocardial infarction (STEMI) status post percutaneous coronary intervention (PCI) will need to be on dual antiplatelet therapy with aspirin and clopidogrel to reduce the risk of stent thrombosis. Gastrointestinal bleeding is the most common serious bleeding complication from using dual antiplatelet therapy. Prophylactic therapy with proton-pump inhibitors is recommended for all patients with high risk for GI bleeding after PCI. This includes patients with a history of peptic ulcer disease or GI bleeding or at least two of the following risk factors: age > 65, concurrent use of another NSAID, treatment with glucocorticoids or anticoagulants, or history of Helicobacter pylori infection. Given this patient’s age > 65 and concurrent use of glucocorticoids, the best next medication to prescribe is a proton pump inhibitor. Furthermore, the use of pantoprazole is preferred over omeprazole with clopidogrel usage due to decreased inhibition of cytochrome P450 2C19.
Prescribing digoxin 0.125 mg daily (A) would be incorrect, as this woman has a preserved ejection fraction following her STEMI and is on appropriate initial medical therapy. Giving rivaroxaban 2.5 mg twice daily (C) would further increase her bleeding risk and is not currently indicated. This patient has a preserved ejection fraction following her STEMI and has no current indication for sacubitril-valsartan 24 mg/26 mg daily (D).
One Step Further Question: What is the recommended duration of dual antiplatelet therapy in patients with average bleeding risk and average risk of recurrent ischemia?
Answer: 6–12 months of dual antiplatelet therapy.
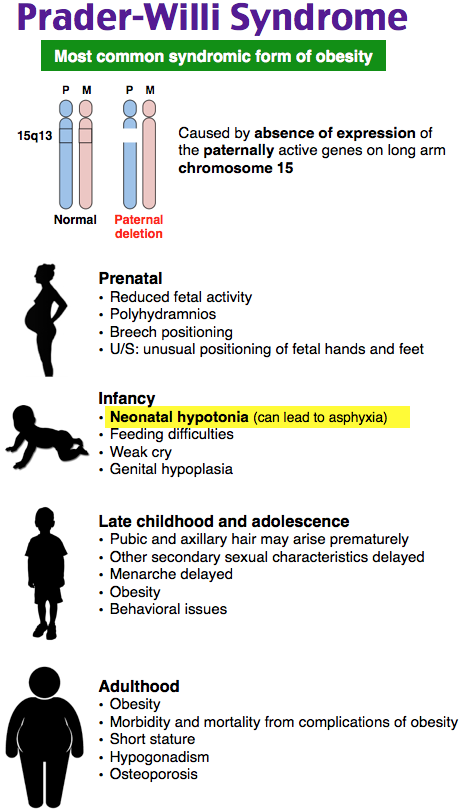
Teaching Images
Here’s a glimpse of a couple of the thousands of teaching images in the Med-Peds Qbank:
Pediatrics
A 4-year-old boy presents to the office for an evaluation of weight gain and lack of satiety after meals. He initially had low tone and difficulty feeding early in life. His parents report that he constantly sneaks food and asks for three times as much food as they would expect each meal. He has thick saliva and snores when sleeping, and his parents report that he has had pauses in breathing during sleep. Which additional physical exam finding would be most helpful in supporting the most likely medical diagnosis?
A) Blindness
B) Microphallus
C) Polydactyly
D) Tonsillar hypertrophy
Answer B
Prader-Willi syndrome is a hypothalamic syndrome and a genetic cause of obesity. It results from loss or inactivation of parenterally inherited genes on the long arm of chromosome 15. Children with this syndrome initially can have decreased muscle tone, poor suck, and feeding difficulties. Within the first 4 years of life, the difficulty feeding transitions first to a normal appetite and then to an increased appetite. Abnormal behaviors surrounding food occur commonly and may include food hoarding, stealing money to buy food, eating from the garbage, eating inedible objects, and a reported caloric intake of three-times the normal for age. This emphasis on eating may result from an increased level of ghrelin, a gut hormone that triggers increased appetite. Continued decreased tone and hypersomnolence may also be present in this syndrome and could result in furthered obesity by leading to decreased tolerance for and participation in exercise. Diagnosis can be made clinically through recognition of major criteria and minor criteria for the syndrome. Evidence of hypogonadism and small genitalia, such as a microphallus, is one of the major criteria for diagnosis. Genetic testing to confirm the diagnosis involves testing for abnormal parent-specific methylation imprinting in the critical region of chromosome 15. Treatment options for Prader-Willi syndrome are limited and tend to focus on improving nutrition, exercise regimens, and targeting detrimental behaviors. Bariatric surgery and growth hormone administration may also be considered.
Optic nerve hypoplasia is also a hypothalamic disorder that typically occurs due to a defect during the development of midline cortical structures. Blindness (A) is a characteristic finding of this condition, and 25% of patients will also have associated endocrine abnormalities. However, significant hyperphagia is not a feature of this disease. Bardet-Biedl syndrome is characterized by obesity, intellectual disability, retinitis pigmentosa, deafness, renal and urogenital abnormalities, hypogonadotropic hypogonadism, and polydactyly (C). While obesity and increased appetite occur in Bardet-Biedl syndrome, the food-seeking behaviors are more typical of Prader-Willi syndrome. Obesity predisposes to sleep apnea, which may be associated with a finding of tonsillar hypertrophy (D). However, sleep apnea can occur in the absence of tonsillar hypertrophy, and in patients with obesity, fatty infiltration of the tongue and neck soft tissue may contribute to airway narrowing. Severe obesity has also been associated with decreased efficacy of adenoidectomies for sleep apnea. While sleep apnea is a minor diagnostic criterion for Prader-Willi syndrome, the presence or absence of tonsillar hypertrophy would not be useful in supporting this diagnosis.
One Step Further Question: What disease is caused by maternal loss of the short arm of chromosome 15?
Answer: Angelman syndrome.
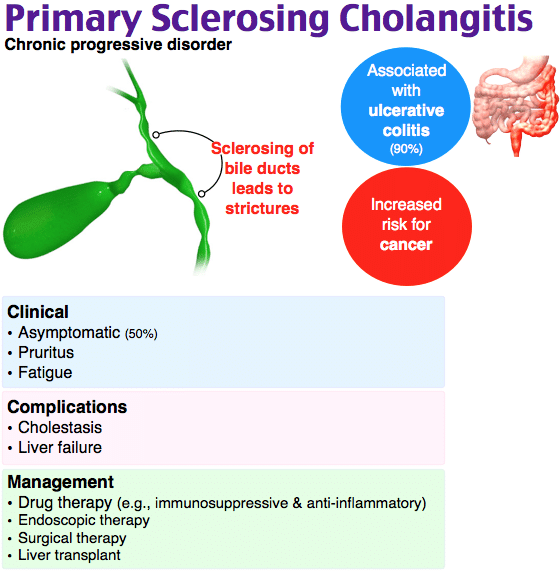
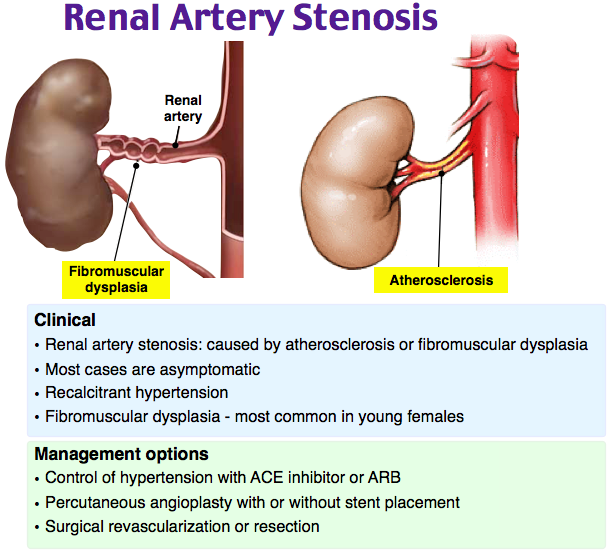
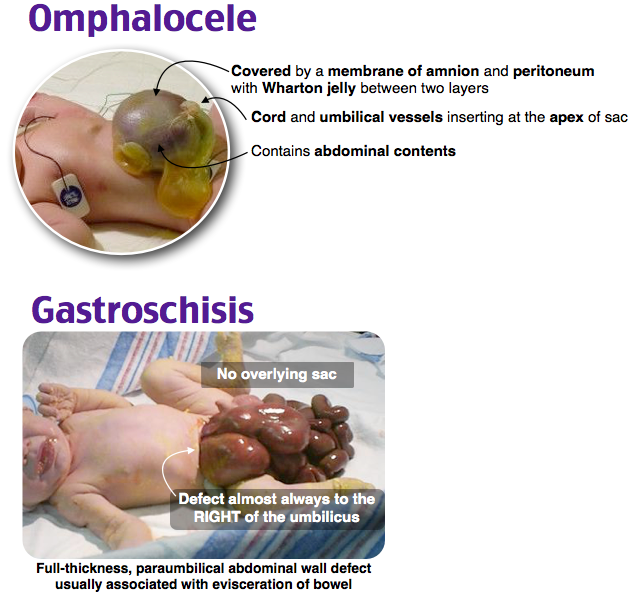
Teaching Images
Here are a couple more of the thousands of teaching images in the Med-Peds Qbank:

As you prepare for your internal medicine and pediatrics board exams, remember Rosh Review is by your side. The Med-Peds Qbank has a Pass Guarantee, so if you don’t pass, you get your money back or extend your subscription for another year at no cost.
Get started with the only Qbank dedicated to Med-Peds. To make sure it’s right for you, try it for free first.
We also offer Pediatric Hospital Medicine Board review from Rosh Review.





Comments (0)